A Model To Prevent Teen Pregnancy
by The Resource Center For Adolescent Pregnancy Prevention
Beliefs and perceptions are powerful forces for every human being. They influence the ways people interact with each other, make decisions about their own behaviors, and plan for their futures.
Adolescents are still in the process of forming their belief systems as they absorb new information about the world around them. In the context of learning about sexual and reproductive health, it’s important to make sure their developing perceptions are accurate.
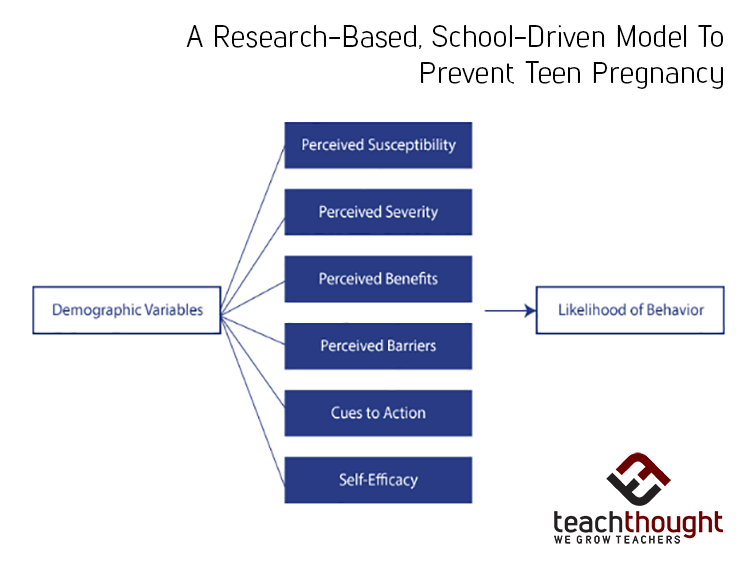
As you plan your high school’s sex education curriculum, the Health Belief Model (HBM) may help you focus on effective ways to influence your students’ perceptions, and as a result, increase their likelihood of taking positive and productive actions for their sexual health.
What is the Health Belief Model?
he Health Belief Model is a framework that presents a series of strategies that help people make better choices about health behaviors.. In general terms, the HBM operates under an assumption that people will take positive, preventative health-related actions if they:
- Feel a negative health condition can be avoided
- Expect specific actions can prevent this condition
- Believe they can successfully take these actions
This model is a way to turn statistics, medical recommendations, and risk factors into concrete, applicable lessons. It can be broken down into six key concepts that will form the foundation of your HBM-based sex education program.
1. Perceived Susceptibility
Do students understand their individual risks of pregnancy, STIs, and HIV? If not, are you able to increase their awareness by personalizing these risks? Use relatable examples to back up statistics about the specific risk factors for their demographic. For example, they may watch videos that feature teenagers of the same race, age, sex, and economic status affected by the risky conditions (pregnancy, STIs or HIV, for example).
2. Perceived Severity
Do students know how serious each condition is? Group discussions and anonymous quizzes are a good way to find out how seriously teenagers take these risks. Your goal is to make sure students understand the personal consequences they will have to face if they don’t take actions to minimize their risks. You may invite guest speakers who learned from their own experiences, or introduce teens to websites that feature other teens facing the consequences of different conditions, such as caring for an infant or taking multiple HIV medications for the rest of their life.
3. Perceived Benefits
Do your students truly understand the benefits of taking steps to prevent these conditions? Do they believe that condoms can prevent pregnancy, and that STI and HIV screenings can prevent health complications from getting worse? Present evidence that your recommended actions will actually benefit teenagers. If they know how effective these strategies truly are, they will be more likely to implement them.
4. Perceived Barriers
What is stopping them from taking this action? The most effective sex education programs will directly address all the obstacles and outside pressures that may affect teenagers’ decisions and perceptions. These barriers can be internal; for example, if a teenager doesn’t think STIs are common, they won’t feel the need to get screened or use protection.
5. Cues to Action
Make sure condom use, STI screenings, and other actionable steps remain in the forefront of your students’ minds. Encourage them to take these steps by providing reminders, tutorials, and up-to-date information throughout the school year. Remind your students to implement the lessons they learned from the program.
6. Self-Efficacy
After teenagers are armed with accurate information about the risks they face, they must believe that they’re capable of taking real and effective steps to prevent them. Positive reinforcement is more effective than scare tactics, because teens need to be confident in their own ability to protect themselves. Teach them how to use condoms correctly, identify the easiest ways to get health screenings, and remind them how capable and empowered they are.
A Brief History of HBM
HBM actually originated in the 1950’s, when three psychologists participated in a tuberculosis (TB) screening program offered for free by the U.S. Public Health Services. Though mobile units created a free and convenient way for people to receive TB tests, it was ultimately unsuccessful because very few people took advantage of the units in their own neighborhoods.
These psychologists created the origins of HBM after studying the people who did choose to get free screenings. These individuals believed TB was a genuine risk, and that the government’s free screenings were effective in reducing that risk. Their heightened perceptions demonstrated the powerful role that perception plays in the actions that people take to prevent health negative conditions.
Social Learning Theories
A few different learning theories fall under the umbrella of HBM, but the following four are the most common and applicable to sex education:
Cognitive Behavioral Theory
Many counselors and psychologists incorporate this theory into their therapeutic approaches, because it teaches patients to identify unrealistic perceptions and change their actions accordingly. The theory focuses on the direct link between thoughts and actions.
Social Cognitive Theory
Learning is a primary part of this theory. It emphasizes the importance of teaching people accurate information, providing sufficient motivation to act upon this knowledge, and empowering them to believe they’re capable of taking the right actions (self-efficacy).
Social Influence Theory
Social norms play a huge role in teenage development, and Social Influence Theory focuses on these influences instead of treating them like inevitable and uncontrollable factors. The theory emphasizes effective ways to actually change social norms in order to change individual behaviors. In the context of a high school classroom, this may mean normalizing safe sex practices and spreading accurate information about risks.
Social Inoculation Theory
This theory focuses on strengthening the individual’s ability to resist social pressures, much like vaccinations strengthen the immune system’s ability to fight off specific viruses. Of course, it requires you to identify the types of peer pressure that may steer teenagers toward misinformed decisions and risky behaviors.
How Can HBM Be Used By High School Health Educators?
When you apply HBM to high school sex education, you must identify the specific conditions and actions that your approach will revolve around.
Conditions
Sexual activity can result in a variety of problematic consequences, but it helps to focus on three specific possible outcomes:
- Pregnancy – Pregnancy affects boys and girls to different degrees, so you will need to acknowledge the specific risk factors for each segment of the population, rather than referencing it as a general risk.
- Sexually transmitted diseases (STDs) or sexually transmitted infections (STIs) – These conditions include chlamydia, gonorrhea, human papillomavirus (HPV), syphilis, and other common diseases, as well as cancer and other conditions that are more likely to occur because of their presence.
- Human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) – Today’s high schoolers weren’t alive during the AIDS epidemic of the 1980’s, but this disease is far from abstract. It’s important to increase awareness of the risks that still exist today.
Of course, the HBM approach also requires actionable steps that students can take in order to decrease their risks and prevent these conditions.
Actions
Preventative actions fall under two categories: primary and secondary prevention. Primary actions actually prevent the conditions, while secondary actions prevent existing conditions from getting worse or spreading.
- Primary actions include the proper and persistent use of condoms as well as other contraceptives.
- Secondary actions include STI and HIV screenings, effective medical treatments, and education about ways to prevent diseases and infections from spreading.
Now that you have the basic building blocks of your HBM-based sex education program, it’s time to implement them into the specific tools and resources you will offer each student.
Incorporate the HBM Checklist into Your Curriculum
Instead of attaching negative connotations to sexuality itself, attempt to educate your students so they can make informed decisions while assessing possible risks.
remember to focus on specific negative conditions and specific actions that teenagers can take to avoid them (or to minimize their consequences). It might help to consult the following checklist as you plan and implement your curriculum:
- Increase perception of vulnerability – Do students realize their risks of pregnancy and STIs?
- Assess perception of vulnerability – Do students understand how severe each condition is?
- Teach the condition and its consequences – Does your program describe specific consequences and risks?
- Assess perception of consequences – Do your students understand how severe these conditions are? For example, do they have a sense of the real struggles associated with parenthood or living with AIDS?
- Present the desired action – Have you outlined the concrete actions that students must take in order to prevent these conditions?
- Assess their belief in this action – Do your students truly believe that using protection and seeking STI screenings will prevent them from experiencing negative consequences?
- Identify barriers to action – Do you know the specific influences that could stop students from taking these actions?
- Eliminate these barriers – Are you correcting misinterpretations and supporting your students’ efforts to resist other barriers, such as peer pressure?
- Provide cues to action – Are you encouraging students to take the right steps?
- Assess their confidence – Do your students believe they’re capable of effectively preventing these conditions?
It’s not enough to teach your students accurate information about pregnancy and STIs; you must also implement ways to assess the effectiveness of these lessons. Solicit feedback, encourage group discussions, and make your program as interactive as possible in order to get an accurate sense of how well it’s working.
Are students becoming more aware of their risks? Have their perceptions actually changed as a result? The most important step is to identify and encourage them to take specific actions to prevent common risks.
Challenges Applying HBM to High School Health Education
Sexuality can be a sensitive subject, especially for teenage students. It’s important to anticipate common challenges that may affect your ability to implement the HBM approach in a high school setting.
Avoiding Victim Blaming
Personal responsibility is one of the main tenets of HBM, but if students are already facing negative consequences of sexual activity, they may internalize this message and feel ashamed. This happens outside the context of sexuality education too. For example, when patients learn it’s their responsibility to take charge of their own health, they may blame themselves for failing to prevent or fix a condition that they already have. When this happens, it’s important to acknowledge that some external influences, such as environmental pollutants or economic circumstances, are outside their control.
Of course, that doesn’t mean you should teach teens to accept this lack of control. Instead, focus on steps they can take to identify and minimize the impact of external threats. Make sure every educator understands that sexual abuse, misinformation, and other uncontrollable factors may affect their students’ ability to prevent certain conditions. Instead of associating negative consequences with blame or failure to act, focus on the steps they can take to minimize future risks.
Continuing Cues to Action
No matter how comprehensive and informative your HBM-based curriculum is, your teenage students will still be flooded with conflicting cues from their peers, the entertainment industry, the Internet, and even their own bodies. With so much misinformation, it’s important to keep your message consistent by providing steady, meaningful, practical cues to action. To increase their effectiveness and make sure you reach every student, you should try to present these cues in multiple ways.
For example, you might deliver information about contraceptive use or STD screenings via posters on classroom walls, newsletter and newspaper articles, school-wide announcements, or other common forms of communication. Of course, parental consent is crucial if you plan to continue sexual discussions outside the classroom. If you only have consent to teach students about potential risks in the context of a sexuality education program, make sure you clarify your ongoing plans with parents.
Using HBM To Empower High School Students
As you guide your teenage students toward positive actions and realistic perceptions, it’s important to remember that each student is an individual who faces unique risk factors and barriers. Be sure to foster an accepting atmosphere so that everyone will feel free and safe to ask questions about the conditions and actions you’ve presented.
Evidence-based, belief-oriented sex education programs are more effective at preventing negative sexual health consequences during high school, but they will also arm your students with the skills and tools they need to make smart choices about their bodies and behaviors for the rest of their lives.
A Research-Based, School-Driven Model To Prevent Teen Pregnancy